NORD supports policies that maximize access to the therapies rare disease patients need by lowering out-of-pocket expenses.
Innovative new treatments and scientific advancements are enabling many patients with rare diseases to live longer, healthier lives. Unfortunately, the cost of these medicines and other treatments that help rare disease patients maintain their overall health can be prohibitive. NORD recognizes that the high cost of drugs has a direct impact on patient access and advocates for policies to lower patient out-of-pocket expenses and maximize access to needed therapies.
A patient’s out-of-pocket costs include their expenses for medical care that are not reimbursed by their insurance. This includes the deductible, which is the amount of money a patient must pay before insurance will pay a claim, copayments, which is the flat dollar amount that a patient pays in addition to a payment made by their insurer, and coinsurance, where the patient is responsible for a percentage of the cost of a prescription as opposed to a flat rate.
For many rare disease patients, their out-of-pocket costs have grown significantly in recent years, as insurance companies are increasingly shifting the cost of prescription drugs onto patients by raising deductibles,1 increasing patient cost-sharing,2 and changing plan design.3 These actions can have grave consequences. Exorbitant out-of-pocket costs can force patients to go without their medication or to use alternative treatments that are not as safe and effective. For example, according to the Kaiser Family Foundation, 26% of all adults’ report difficulty affording their prescription drugs. Of those who were unable to afford their drugs, three in ten say they have not taken their medicine as prescribed due to cost.4
In recent years, there has been a push in state legislatures to assist patients with increasingly high prescription drug out-of-pocket costs, and states have explored different types of legislation with varying impacts on patients’ out-of-pocket spending. It is important to note that state lawmakers do not have authority over all forms of health insurance. For the purposes of this report, the analysis of out-of-pocket cost protections focuses solely on state-regulated health insurance plans.
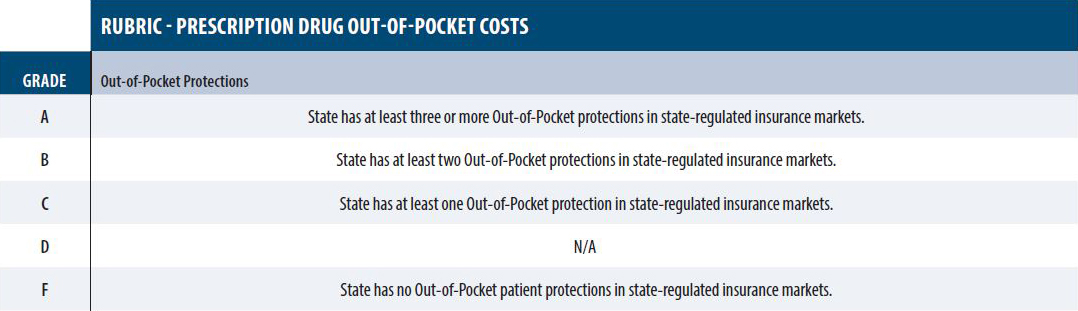
NORD evaluated state out-of-pocket patient protections on the following:
The greater the number of protections states have enacted from above, the higher their grade.
Click to enlarge